Naptics: Convenient and Continuous Blood Pressure Monitoring during Sleep
Andrew Carek and Christian Holz. IMWUT 2018.
Microsoft Research, Redmond, WA.
Figure 1
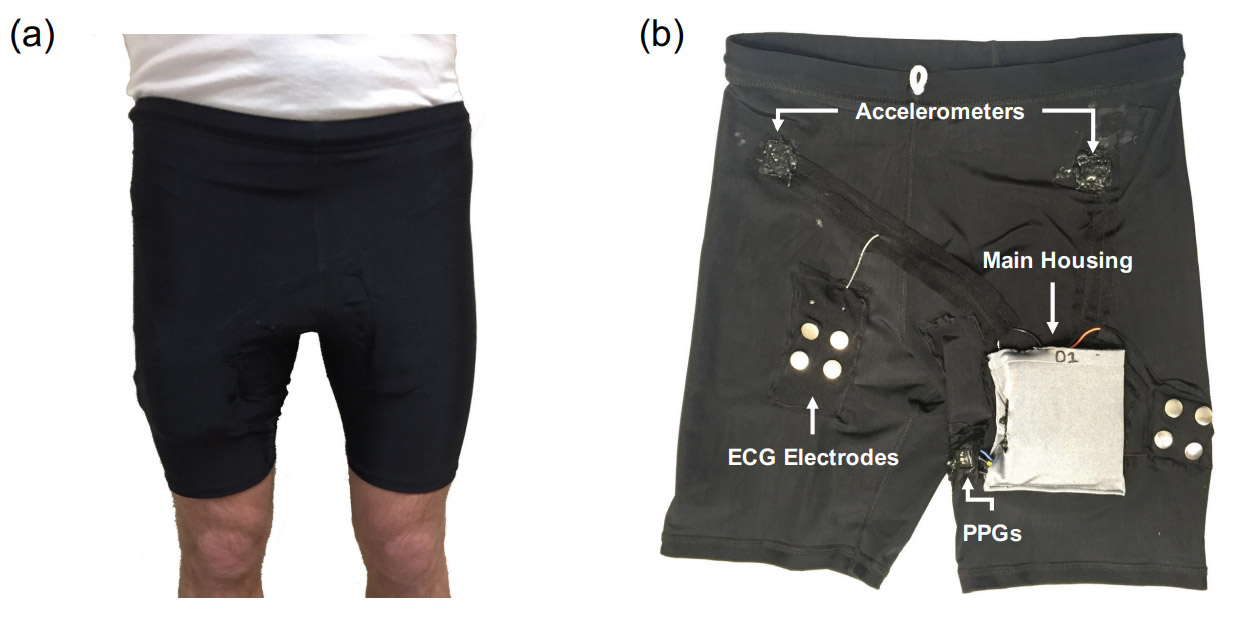
a) Naptics is a wearable device woven into a pair of compression shorts to continuously monitor the wearer's blood pressure during the night. b) Naptics incorporates a series of physiological sensors, including electrocardiogram (ECG), ballistocardiogram (BCG) using sensitive accelerometers, multiple optical photoplethysmography (PPG) sensors, as well as a pulse oximeter and a temperature sensor. Naptics continuously records the measurements of all sensors and derives the wearer's pulse transit time, a metric that correlates highly with a person’s blood pressure. Naptics saves all records on a storage card along with timestamps from a real-time clock.
Abstract
Normal circadian rhythm mediates blood pressure during sleep, decreasing in value in healthy subjects. Current methods to monitor nocturnal blood pressure use an active blood pressure cuff that repeatedly auto-inflates while the subject sleeps. Since these inflations happen in intervals of thirty minutes to one hour, they cause considerable sleep disturbances that lead to false measurements and impact the person's quality of sleep. These blood pressure samples are also just spot checks and rarely exceed 10–15 values per night.
We present Naptics, a wearable device woven into shorts. Naptics passively monitors the wearer’s blood pressure throughout the night—continuously and unobtrusively—without disturbing the user during sleep. Naptics detects the micro-vibrations of the wearer's body that stem from the heartbeat and senses the optical reflections from the pulse wave as it propagates down the wearer's leg. From the timing between these two events, Naptics computes the pulse transit time, which correlates strongly with the user's blood pressure.
Naptics' key novelty is its unobtrusive approach in tracking blood pressure during the night. Our controlled evaluation of six subjects showed a high correlation (r = 0.89) between Naptics' calibrated mean arterial pressure and cuff-based blood pressure. Our in-the-wild evaluation validates Naptics in tracking five participants' blood pressure patterns throughout four nights and compares them to before and after cuff measurements. In a majority of the nights, Naptics correctly followed the trend of the cuff measurements while providing insights into the behavior and the patterns of participants' nocturnal blood pressure. Participants reported high sleep quality in sleep diaries after each night, validating Naptics as a convenient monitoring apparatus.
Publication

Contributions: Cuff-less passive nocturnal blood pressure monitoring
- A technique to continuously record the wearer's pulse transit time through simultaneous monitoring of BCG and PPG during sleep, which records cardiac events at a proximal and a distal location, respectively. The resulting measurements of nocturnal PTT give insight into the wearer's night-time hemodynamics and can assist in diagnosing hypertension, managing medications, or determining cardiovascular risk.
- Naptics, a prototype device that unobtrusively integrates with a convenient shorts-based form factor and that does not interfere with normal sleeping patterns. This increases the reliability of true nocturnal measurements compared to cuff-based disruptions. Naptics also integrates physiological sensors such as temperature and pulse oxygenation that are useful in monitoring sleep behavior and quality.
- Two evaluations that establish the feasibility of our method and prototype in a six-participant controlled lab evaluation and that demonstrate the promise of our approach during a five-participant in-the-wild evaluation over the course of four nights, resulting in insightful and fine-grained blood pressure patterns, all while participants rated sleep quality as high in sleep diaries.